Glossary
|
4 hrs, 3 times/week |
This is a vital note: Throughout the world, in nearly every dialysis service, 4 hours of dialysis 3 times per week is 'standard treatment'. In some places, particularly in the US, treatment times have been significantly less than 4 hours while in some European, Japanese and Australian centers, 5 hours is more common .... but there is no escape from the general principle of the 3 x 4 dialysis treatment concept. |
|
4-5hr x 3/week |
Predominant current dialysis practice is built around providing (funding) dialysis 3 times per week and for an average of 4-5 hours per treatment … though in some places, it may even be less than this. |
|
4x3 |
Throughout the rest of this web site, you will find the current prevalent dialysis practice referred to as 4x3 (for 4 hours, 3 times per week) |
|
Adequate |
Adequate: is defined as 'satisfactory' or 'enough for what is necessary' |
|
Aldosterone |
Aldosterone is a hormone, produced by the adrenal gland, which is produced after the kidneys release renin. Aldosterone acts back on the kidneys to cause salt and water to be retained in the body. It thus contributes to the rise in blood pressure and the retention of fluid that often accompanies kidney trouble. |
|
Back-slabs |
If desired, a plaster or, better, a light-weight molded plastic forearm back-slab (like injured footballers use) can be molded by your hospital orthotics department to provide both support and protection for the fistula. It can also be designed to have a Velcro-fastened 'protector' cage to cover the fistula and to provided added protection against inadvertent damage when rolling over at night. We have not used this concept as we have not found it necessary, but it is an option if patients are anxious about added access protection whilst asleep. |
|
Blood access |
Haemodialysis depends on access to the blood circulation so that blood can be removed, run through the dialyzer, cleansed, and returned back to the body. This is done either through a fistula (the preferred method) or by the use of a catheter (soft, wide-bore tube) inserted into a large vein - commonly the jugular vein at the base of the neck. In NHD, either can be used though we prefer the fistula. A fistula is where, with a small operation, an artery and vein are joined together, commonly at the wrist or elbow, to increase the pressure in and size of the vein so that easy needling is possible and higher blood flow rates can be obtained. |
|
Blood flow rate |
This simply refers to the rate at which blood is pumped out of the body and through the 'dialyzer' (see below). The faster the rate, the more blood can be passed through the dialyzer and 'cleansed' of wastes. High flow rates may not, however, be a 'good thing' for the circulation and the blood access (see later). NHD allows more effective dialysis but at lower blood flow rates - thus making dialysis an altogether more gentle and 'friendly' process. |
|
Body salt and water |
The kidneys control the amount of salt and water in the body. This, in turn, influences the volume of blood in the blood vessels and in the tissues of the body. Too much, and the blood pressure rises, the heart labors and the legs and lungs get 'water-logged'. Too little, and the tissues get dry, thirst and dizziness occur and the urine output falls. Regulating the correct proportions of salt and water (or getting the blood volume and tissue fluid content right) is one of the most important things the kidneys do. |
|
Calcium deposits in blood vessel walls |
As a result of problems with calcium and phosphate control (which is beyond the scope of this website to explain in detail), calcium is often deposited in the walls of arteries. This causes the arteries to become stiffened and for blood flow through them to be reduced. This in turn may compromise the blood flow, especially to the heart muscle and to the lower limbs. It may even lead to loss of limbs through the development of dry gangrene (loss of blood supply) and the need for amputation. NHD has been shown not only to prevent 'calcification' of blood vessels, but actual re-absorption (reduction) in the calcium deposits already formed. |
|
Center-based haemodialysis |
In-center dialysis is commonly performed, at least here in Australia, in large, hospital-based dialysis units. Here, most or all of the treatment is provided by trained dialysis nursing staff, supervision levels are high and patient 'participation' and self-reliance is minimal. Dialysis schedules are rigid and are designed to fit the convenience of the center rather than the individual patient. |
|
Chemical wastes |
These are described in some of the 'links' but include nitrogen-based wastes like creatinine and urea, food wastes like phosphate, acid wastes generated by the body's energy processes and a host of other toxic substances made every day by the body which. if not eliminated through the kidneys, build up to poisonous levels and make us sick. |
|
Chronic kidney failure |
The causes of chronic kidney failure are described at http://www.kidneywise.com/basics/kidneys/causes.asp. Though the incidence (the frequency of one cause relative to another) varies from country to country, diabetes, high blood pressure and inflammation of the kidneys (nephritis) are the three commonest causes in all countries. For more information on the causes of kidney failure just click here for lots of useful sites. |
|
Connector boxes |
Small plastic molded locking boxes can be fitted over the connections between the dialysis blood lines and the access catheter limbs to prevent disconnection. These need to be made to fit the particular catheter type in use but this can be done simply and cheaply and, as they do not need to be sterile, they are reusable. |
|
Daily, short-hour, 5-7 days/wk |
Some centers are using shorter hour treatments - but more of them. Six two hour treatments/wk are usually given - with some significant advantages when compared to three four hour treatments/wk, even though the number of hours per week are the same. |
|
Dialysis |
The medical term to describe 'artificial kidney treatment'. Do you want to know how dialysis works? |
|
Dialysis fluid (dialysate) flow rate |
The dialysis fluid is a carefully constructed fluid which comes into contact with the blood separated only by the dialysis 'membrane'. It must be ultra-pure and the concentration of the several salts it contains carefully controlled. It is constantly being replaced and, as it is, wastes are constantly 'washed away' out of the blood stream. See our How Dialysis Works page for more information on this topic. |
|
Dialysis membrane surface area |
This is the area (usually expressed in square meters) that the dialysis membrane would occupy if it were rolled out and 'flattened'. The bigger the membrane, the greater the area for waste 'transfer'. Increasing the membrane size is one of the ways by which dialysis efficiency can be enhanced. |
|
Dialyzer |
The medical term for the 'artificial kidney' - the filter that 'dialyzes' (removes waste from) the blood. |
|
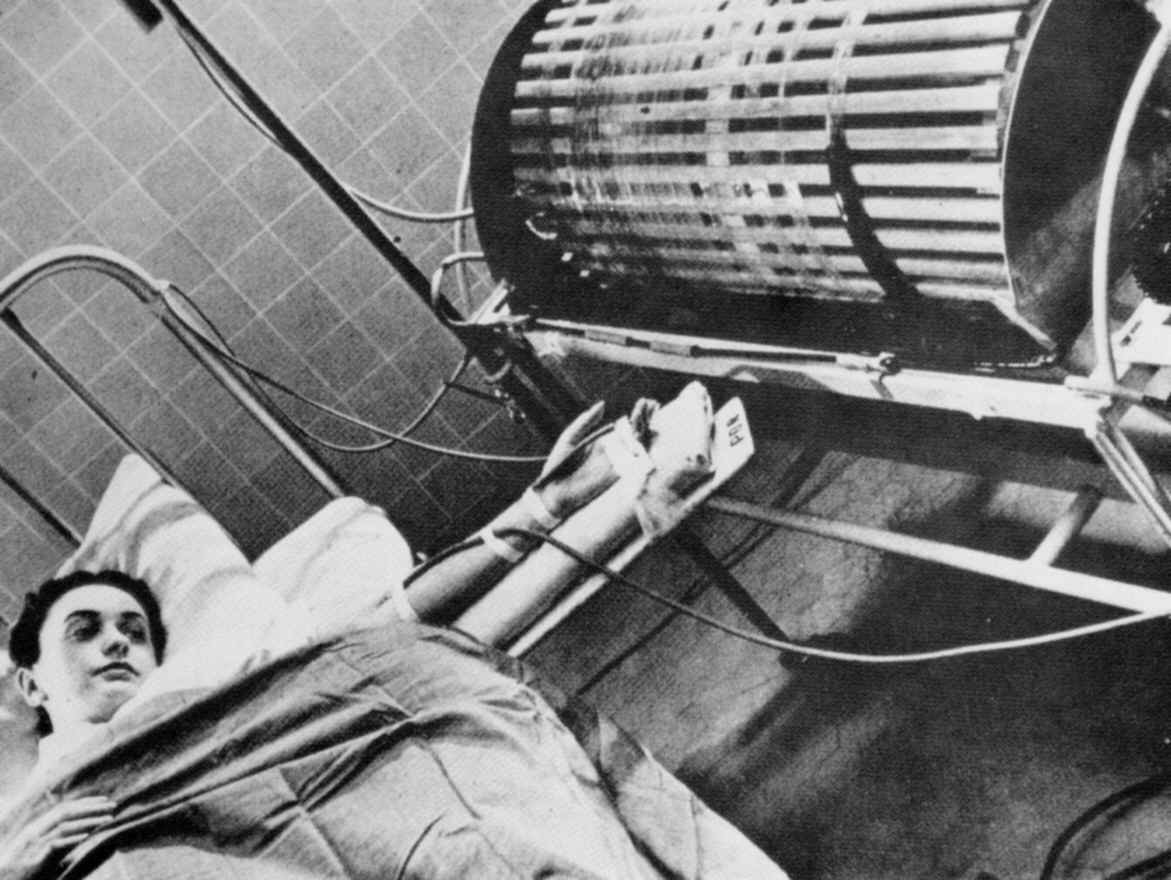
Early dialysis machines |
|
|
Electrode impregnated mat |
A mat (like a bed-wetting mat) placed under the machine. It has two electrode strips woven through (like in an electric blanket), one +ve and one -ve. If the mat is wet by a leak from the machine, a current flows through the wet mat between the electrodes, completes an electrical circuit and sets off an alarm. |
|
Electrode impregnated tape |
Just like the electrode-impregnated mat under the machine, we use a light cloth tape - also with electrode wire imbedded in it - which is loosely looped around the access arm or placed under the catheter connection sites before sleep. If blood seepage occurs from either site (depending upon the access used), an alarm is triggered. We had some teething problems with this warning device - it was so sensitive that normal body sweat was sufficient to set it off. Putting a layer of gauze under it has solved the problem. |
|
Erythropoeitin |
Erythropoeitin (called EPO for short) is a very important hormone made by the kidneys. It is responsible for 'telling' the bone marrow (the factory where red blood cells are made) to make red blood cells. No EPO - no red blood cell manufacture. In kidney disease, the ability to make enough EPO falls. As EPO production falls, so too does the manufacture of red blood cells in the bone marrow. This results in a low red blood cell count (anemia) - which is a feature of almost all kidney disease and is the main cause of the lethargy and weakness which accompanies kidney trouble. |
|
Frequency |
Frequency of dialysis means the number of times the treatment is carried out in a week. |
|
HD |
Throughout the rest of this web site, you will commonly find haemodialysis referred to as 'HD.' |
|
Haemodialysis |
One of the two main varieties of artificial kidney treatment (the other is 'peritoneal dialysis'). These will be explained in more detail within the text as you move through this web site. |
|
Heparin |
An anticoagulant - a drug which prevents the blood from clotting and which is needed in dialysis to prevent clotting as the blood flows out of the body and through the dialyzer. |
|
Home-based haemodialysis |
Home haemodialysis is encouraged and supported in some countries more than in others. In home dialysis, the patient is taught to take all responsibility for routine dialysis care and dialyze in their own homes and at their own convenience. Home haemodialysis removes the problems of transport to and from the center, reduces operating costs, allows for flexibility and freedom to dialyze according to the patient's schedule and not that of the center and, perhaps most importantly of all, encourages pride and self-esteem through self-care and self-responsibility. |
|
Inversely related |
An inverse relationship is when, like a seesaw, as one 'thing' rises, another thing must fall. In the context of dialysis, as the speed and aggressiveness of the process rises, the outcomes (measured as health and well-being) decline. This has been shown in all and every study. |
|
Kiil plates |
Kiil plates were the original dialysis 'membranes' and were not unlike the filter vanes that are inside a swimming pool filter ... they had to be disassembled after each dialysis treatment, cleaned, and reassembled. It was a grueling task. Modern hollow fibre dialysers are a far cry from those early days, but the principles are unchanged. |
|
Kt/V |
Kt/V is the name given (don’t ask me to explain why) to a complex mathematical calculation of dialysis adequacy. In very, very simple terms, it describes the amount of waste removed from a 'given' volume of the body fluids in a 'given' time by a membrane with 'given' characteristics. All I can say is I believe it is a flawed concept. It has dominated our thinking, though, for 20 years ... and in the process, blinded us to the real truth - that dialysis adequacy cannot be expressed by math or a number, but depends on far, far more basic concepts ... time and frequency. |
|
Left ventricle |
The main pumping chamber of the heart - which thickens ('hypertrophies') in kidney disease and kidney failure under the triple influences of high blood pressure, excess blood volume from fluid retention and anemia. |
|
Length |
Length of dialysis means simply the number of minutes (or hours) of any given treatment. |
|
Limited care 'satellite' haemodialysis |
In limited care centers, the patient is encouraged and taught to perform some, most or all of the dialysis treatment, taking as much responsibility for their own treatment as is possible. Here, supervision levels are lower and self-reliance is encouraged. Dialysis schedules are still center-oriented and only limited flexibility is possible for individual patients. |
|
Logged numbers |
The phone numbers of key support staff are logged into the memory of the bedside phone so that easy contact is possible through the night is help is needed. |
|
Long, slow, nocturnal 3.5 nights/wk |
By dialyzing through the night, dialysis hours can be extended without disrupting daytime activity. By extending dialysis hours, therapy can be more gentle and more efficient, clearing more waste but at a slower rate. Dialysis every 2nd night (or 3.5 times a week) for an average of 8-9 hours per session extends dialysis time from the usual weekly 12 hours to ~30 hours/week. |
|
Long, slow, nocturnal 6-7 nights/wk |
In my view - by far and away the optimum dialysis regime. In this option, dialysis time is extended from the usual 12 hours per week to 50-60 hours per week …. Yet the waking hours remain free and untroubled by dialysis commitments. This concept is what this whole web site is devoted to exploring with you - so, if this makes sense to you …. read on! |
|
Mean Kt/V of 1.3, 3 times/wk |
This is a complex concept - but if you remember the description of Kt/V (see above), you will remember that dialysis adequacy (how I dislike that mediocre term) is calculated by a formula (Kt/V) to produce a 'magic' number. The magic umber for 'adequate' dialysis is a Kt/V of 1.3. Just accept that that is so ... its far too complicated to explain in detail. 4x3 HD should, to be 'adequate', yield a Kt/V of 1.3 each dialysis - or, for 4x3 HD, three times per week. |
|
Ml/min |
The abbreviation ml/min = milliliters per minute. When applied to kidney function - often called 'clearance' (or the ability of the kidney to clear (or remove) waste from the blood stream) - it signifies the amount of blood 'cleared' of waste (e.g.: creatinine) in a given time. Normal kidney function or 'clearance' of 100 ml/min means that 100ml of blood can be cleansed of waste by two normal kidneys every minute. 4x3 haemodialysis gets nowhere near this, clearing only 13 ml/min. NHD can achieve 4 times the clearance of 4x3 HD with ~ 50 ml/minute cleared of waste. |
|
Modem/internet technology |
The first NHD group from Toronto have used modem and internet monitoring to 'watch' their patients through the night. Most NHD units now do not modem-monitor … though the option is there. It certainly adds to the cost of setting up a program and the Toronto group maintain that were they setting up now with the knowledge about the program they now have, they would not install modem monitoring. |
| Mupirocin ointment | Mupirocin ointment is a topical antibiotic or bacteriocidal. Mupirocin prevents bacteria from growing on the skin. It is particularly helpful against staphlococci. |
|
Optimum |
Optimum: is defined as 'best'. |
|
Other centers around the world |
Longer and more frequent dialysis is not new. The earliest recurrent dialysis programs in the 1960's were all 8-10 hours long. Dr Charra in Tassin, France, has continued this style of dialysis to this day - with consistently the best patient outcomes published anywhere. Long and more frequent dialysis (nocturnal, through-the-night dialysis) was pioneered in Toronto by Drs Uldall and Pierratos - with several others following their lead (including ourselves) ...... but more of that later - it is, after all what this website is about!) |
|
Osteoporosis |
Osteoporosis is when the bones get slowly weakened by the removal of their calcium. There has been some concern that heparin, which can leech calcium from bone, may promote osteoporosis over time, especially in NHD where the exposure to heparin is significantly greater due to the significant increase in dialysis time. To date, careful studies by the Toronto group have failed to confirm this fear and bone strength appears to increase rather than decrease with time. |
|
Peritoneal dialysis |
This is the second main option in dialysis. It is not the province of these notes to deal with this choice but there is a nocturnal choice in peritoneal dialysis too - 'automated peritoneal dialysis' - which our unit has embraced also for the 25% of our dialysis population who choose peritoneal dialysis as their preferred dialysis method. I suggest you visit the suggested website as a first step if you wish to know more of this choice. |
|
Phosphate binding medications |
One of the biggest problems for patients on dialysis is the inability to remove enough phosphate from the body. 4x3 HD isn't efficient enough to remove it so 'phosphate binders' are used … drugs like sevelamer (renalgel) or calcium carbonate, which bind (or 'lock on to') phosphate inside the bowel and convert it into a form which cannot be absorbed into the body. As a result, it passes out in the motions. The problem is, dialysis patients often have to take 'truckloads' of the stuff - and they can cause constipation and other problems. NHD removes so much phosphate that not only are binders no longer required, but phosphate may need to be added to the dialysate fluid to sustain body levels. |
|
The period of renal failure where kidney function is very low and dialysis preparation should be well underway. |
|
|
Provider |
Provider' refers to your hospital, dialysis service or local health provider ... those with the responsibility for funding the dialysis program - though ultimately governments fund at state of national levels. |
|
Qd = 100 ml/min |
"Q" if used in dialysis language to represent 'flow rate' of a fluid - be it blood or dialysate. Qd refers to the flow rate of the dialysis fluid (dialysate) past the dialysis membrane (or through the dialyzer). A Qd of 100 ml/min, the rate used in early NHD is 1/5th or 1/6th that used in conventional 4x3 HD - yet it still allowed huge increases in dialysis efficiency because of the increase in dialysis time and frequency. |
|
Qd = 300 ml/min |
Qd = 300 ml/min means (see the explanation for Qd = 100 ml/min) that the dialysate flow rate is passing through the dialyzer at a speed of 300 mls every minute. |
|
Renin |
Renin is a hormone made by the kidneys. By a rather complex pathway, renin release leads to a rise in blood pressure in two ways: (1) it stimulates the production of 'angiotensin II' (or A II) which constricts (or squeezes) small arteries and (2) it stimulates the production of the hormone 'aldosterone' which causes the kidneys to retain salt and water. The combined effect is to have smaller blood vessels containing a bigger volume of blood - and the blood pressure therefore rises. |
|
Short, aggressive |
These terms will be clearer as the web site unfolds but…... 'short' refers to the hours spent on the dialysis machine; 'aggressive' means the rate at which fluids and wastes are removed within the dialysis treatment time. 'Short, aggressive' means the most rapid removal of fluids and wastes in the shortest time possible - it seems appealing, but very, very hard on the human body. |
|
Sleep apnoea |
A condition common to dialysis patients especially, where, linked with snoring, oxygen levels to the brain drop at night and there are periodic pauses in the breathing cycle during sleep. It is associated, among other things, with poor sleep quality and day-time drowsiness. It responds well to NHD and sleep quality improves as a result. |
|
Standard, conventional forms |
For decades now, haemodialysis has been shackled within rigid programs more designed to fit staff schedules and enhance profit margins than to provide good outcomes for the patient. The prevalence of so-called 4x3 programs (4 hours treatment, 3 times per week) around the world attest to this. These rigid and brief dialysis programs are not, however, always in the patients' best interests. |
|
The buttonhole technique |
A technique for insertion of dialysis needles where the same insertion site and track is used repeatedly. |
|
The meter2/hour hypothesis |
An early concept in dialysis lore: in essence, that time on dialysis can be reduced if the size of the dialysis membrane (see below) is increased. |
|
The significance of "adequate" |
There is a whole 'industry' in dialysis based on the word 'adequate'. The effectiveness of dialysis is measured by mathematical formulae like Kt/V (you will meet this again later) or by blood-based calculations like Urea Reduction Ratio (again, later) - all designed to determine if the dialysis treatment is adequate. But 'adequate' implies by definition that there is better ... so, would you really opt for 'adequate' when optimum was possible? |
|
Vitamin D |
Vitamin D is converted in the kidneys from the inactive vitamin substance we absorb from food through the gut into its 'active' form. 'Activated' vitamin D promotes the absorption of calcium by the gut from the food we eat. This calcium is needed to maintain healthy bones. In kidney disease, the kidneys cannot 'convert' sufficient vitamin D. Calcium absorption therefore falls and blood calcium levels fall. Low blood calcium levels cause the release of a hormone, parathyroid hormone, from 4 small glands in the neck. This hormone frees calcium from bones to maintain the blood calcium levels but at the expense of weakening the bones. |
Authored by Prof John Agar. Copyright © 2012
Nocturnal Haemodialysis Program, Barwon Health.
All rights reserved. Revised: July 1st 2012